Means of Egress - Clinical Impact
This content includes information linking Environment of Care and Life Safety Code deficiencies and their impact on patient care and patient safety.
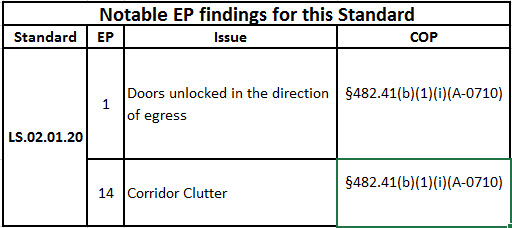
LS.02.01.20: The organization maintains the integrity of the means of egress
Means of Egress: Clear and unobstructed
Clinical staff must have a basic understanding of the means of egress. Keeping the corridors clear of obstructions is important for several reasons: (1) fire rescue, (2) employee health and safety, and (3) compliance with the Joint Commission and CMS.
Fire Rescue
Compliance with the Life Safety Code is not an option for your organization but a requirement. This code clearly requires the egress corridor to be clear and unobstructed. The Life Safety Code “establishes minimum criteria for the design of egress facilities so as to allow prompt escape of occupants from buildings, or where desirable, into safe areas within the building.” (NFPA 101-2012, 1.1.3) Healthcare buildings have established that an 8 foot wide corridor is optimal, allowing for two hospital beds coming and going to pass while transporting patients. This corridor must be clear to allow for this bed movement. Following de-briefing with clinical staff following catastrophic events, we often hear that staff with clear corridors were successful in rescue, but those that admitted corridor clutter shared the problems of trying to navigate around the equipment while trying to perform rescue.
Often staff state that they cannot be bothered with putting equipment away, or that by leaving equipment in the corridor it is easily accessible later when it is needed. Nonetheless, this equipment, when left in the corridor, creates difficulty when moving patients during normal operations. When moving a patient from one location to another, it is difficult to turn the bed to avoid equipment. During an emergency, this becomes much more difficult. Not having to wheel a patient around equipment in the corridor has proven to save lives in emergencies.
Employee Wellness
Staff carrying equipment may accidentally bump into equipment improperly stored in the egress corridor, causing injury or dropping the items being carried. Staff injuries may reduce effective staffing levels, cause discomfort to staff during healing, and possible compensation claims. Dropping equipment may be loud and disturbing to patients in the area, or damage the items being carried.
Corridor clutter can have a substantial impact on the health and safety of our patients and workforce. Additionally, healthcare employees who get injured on the job are less productive, less attentive, more susceptible to further injury, and may be less likely to deliver safe patient outcomes. Corridor clutter is a shared responsibility. Creating a “safety always” environment and minimizing known risks can advance employee health and safety while creating a safe environment to care for patients.
The “Safety Always” culture is where equipment and supplies have a designated safe place to be stored within the clinical units. The key to this is holding the clinical team accountable for making sure equipment and supplies “always” gets to the safe/appropriate destination. This also includes engagement from support staff who may visit the area/department to drop off supplies. One strategy that can be used to monitor and sustain this practice over time is to include a “daily storage report” at the team huddle or department meeting.
Advance planning can help reduce corridor clutter. Assigning storage space for equipment and training staff to store equipment appropriately will reduce noncompliance.
Compliance
The Joint Commission and CMS, as authorities having jurisdiction who have adopted the National Fire Protection Association Life Safety Code, include enforcement is part of accreditation. CMS has adopted the NFPA codes by statute, which is why issues like compliance with the Life Safety Code is not an option but a requirement.
It should be noted that the Joint Commission allows crash carts to always be in the means of egress, as they are always in a stand-by mode. There is no requirement to have these plugged into receptacles that are also powered by the emergency generator, although this may be best practice. Isolation carts and Chemotherapy carts are also allowed in the means of egress while associated with a specific patient.
Staff carrying equipment may accidentally bump into equipment improperly stored in the egress corridor, causing injury or dropping the items being carried. Staff injuries may reduce effective staffing levels, cause discomfort to staff during healing, and possible compensation claims. Dropping equipment may be loud and disturbing to patients in the area, or damage the items being carried.
Means of Egress: Door locking
In healthcare, doors are locked for specific reasons, and under specific circumstances. Restricting access to areas like medication rooms or storage areas with hazardous materials (such as radiology and storing radioactive materials in the hot lab) are reasons for door locking. Protecting patients by locking units to restrict access, such as pediatrics or the obstetrical units often occurs. Restricting patient movement by locking patient rooms and egress from the unit, such as behavioral health care and Alzheimer’s units are other areas where doors are locked. In each of these settings specific criteria exists based on fire safety principles. In locked units all staff must carry the key to facilitate egress in an emergency; only authorized staff have keys to certain hazardous storage rooms like the hot lab in Radiology. Delayed-egress doors have a time delay before they open, allowing staff to respond to a patient attempting to elope or leave a unit without staff permission. Access-controlled doors restrict unauthorized people from gaining entry.
The Joint Commission expects all staff affected by door locking to understand why the locking is required and how to unlock the doors in an emergency. The provision that when locking patients behind a door all staff carry keys to facilitate emergency egress is rooted in patient safety. History has shown that when doors are locked and staff did not have keys readily available, lives are lost. For example, 41 people lost their lives in a 1950 fire in Davenport, Iowa. The report stated that “due to the locked doors … and the lack of prearranged procedure for evacuation of the building in case of an emergency, it was possible to rescue only 25 of the 64…” Granted that this was many years ago, but the fact that locked doors contributed to a lack of rescue still occurs.


